Medical Ketogenic Diet Therapy
We review the range of diets and conditions they treat
What is a ketogenic diet?
A ketogenic diet is very high in fat and low in carbohydrate. Adequate protein is provided to ensure typical requirements are met. This is especially important for children who continue to grow and need sufficient protein to facilitate this.
It’s surprisingly easy to exceed our protein requirements, so for most individuals, starting a KD will involve a reduction in protein intake alongside a significant decrease in carbohydrate and increase in dietary fat intake.
KD therapy encourages the brain to switch its preferred fuel source from glucose to ketones. When we consume carbohydrates like bread, rice, pasta, fruit, and vegetables, these are broken down to produce glucose, which the brain usually uses as energy. However, the brain is also capable of using ketones as an energy source.
With KD therapy, carbohydrate is significantly limited, so the high dietary fat intake is broken down to produce ketones: acetoacetate, beta-hydroxybutyrate and acetone. The brain can use these ketones as an alternative fuel source to glucose. Fat is very filling and satiating, so the individual feels full despite the occurring metabolic shifts. Clinical and research data clearly demonstrates the effectiveness of KD therapy, but the underlying mechanisms are as yet not fully understood.
Types of medical ketogenic diet therapy
There are five main types of KD:
- Classical KD
- Medium-chain triglyceride KD
- Modified KD
- Modified Atkins KD
- Low glycaemic index treatment (LGIT)
These are examples of medical KD therapy, individually calculated, prescribed, and monitored by a specialist dietitian for each client. Not to be confused with lower carbohydrate diets that some individuals might undertake for weight loss. Lower carbohydrate diets contain anywhere between 50-130g of carbohydrate per day. In contrast, a medical ketogenic diet often has 10-20g of carbohydrate per day depending on the individual and type of KD prescribed.
Now let’s examine each diet in more detail…..
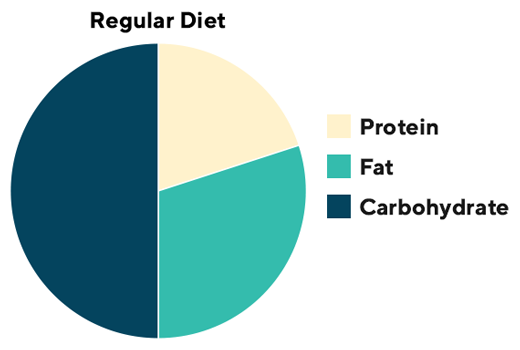
Regular Diet
First lets start with a regular diet. A typical western diet predominantly consists of carbohydrate (50%) and protein (15-20%), with lower energy coming from fat (30-35%). We generally don’t tend to count, weigh, or track our food and drink intake. Instead, eating essentially what we wish but ideally following public health guidance like the Eatwell Guide in the UK or similar in other countries. In contrast, strict adherence to the prescribed KD is essential to ensure ketosis is sustained. Some handy measures and portions can be used for ease, but foods are often weighed to ensure accuracy.
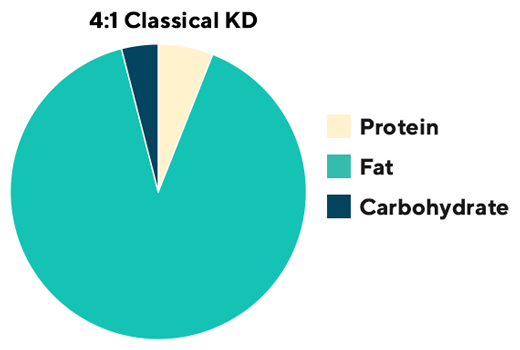
Classical Ketogenic Diet
The classical KD is calculated and prescribed in ratios. The highest ratio (4:1) is lowest in carbohydrate and highest in fat; 4g of fat for every 1g of carbohydrate plus protein equating to about 4% of total energy from carbohydrate. Long chain triglyceride (LCT) fats such as butter, cream, oil, and mayonnaise dominate.
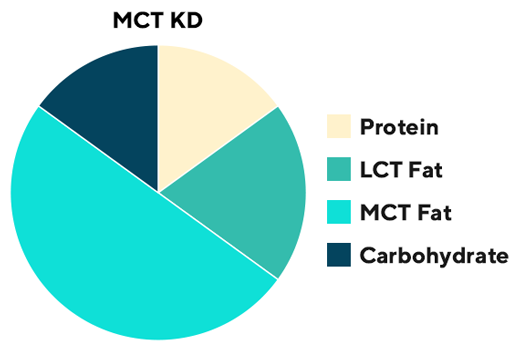
The MCT Ketogenic Diet
The medium chain triglyceride (MCT) ketogenic diet is so-called because a significant percentage of the fat prescription (30-60%) comes from MCT fat sources like MCT oil and coconut oil. MCT fat is absorbed and transported more efficiently than LCT fat, resulting in a greater yield of ketones. Therefore, less total fat is needed, and users can have a slightly higher carbohydrate (up to 18% of energy prescription) and protein intake. MCT fats can cause gastrointestinal side effects, so intake is monitored and fine-tuned according to tolerance. Both the classical and MCT KD demand that all foods are weighed and measured precisely.
Modified Ketogenic Diets
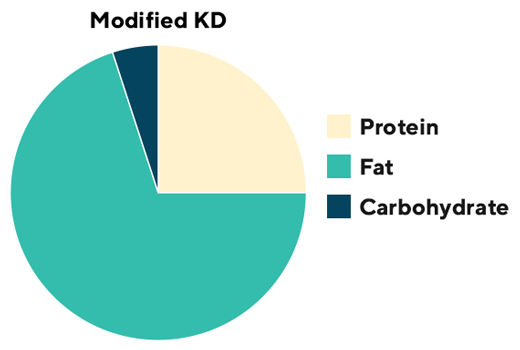
Modified KDs encompass the 1) Modified Atkins Diet (MAD) protocol and 2) the Modified KD. They are often described as hybrid KDs as they adopt principles from the classical and often MCT KD protocol but are more flexible. In general, 10-30g of carbohydrate (or 5% of total energy) are typically prescribed daily, together with 60-80% fat and moderate protein.
The Modified Atkins Diet (MAD) protocol is very flexible, where grams of carbohydrate are prescribed, liberal fat is encouraged with every meal or snack and protein intake is flexible.
The Modified KD is slightly less flexible as grams of carbohydrate AND fat are prescribed and measured but protein intake is less strict.
Low Glycemic Index Treatment
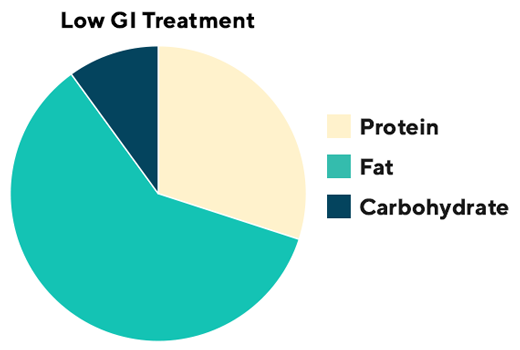
First described in 2005, LGIT restricts daily carbohydrates to 40-60g (including fibre) but only those with a glycaemic index of less than 50. Foods are not weighed but typical portions are used.
Which ketogenic diet is most popular?
We undertook a systematic scoping review of the literature over a ten-year period and identified that the classical KD is the version most frequently used in research studies. Yet, interestingly, in clinical practice we use all diets but especially those which are more liberal than the very strict classical KD. In a survey of ketogenic dietitian’s in the UK and Ireland, the modified KD was reported to be used most often. So how does your dietitian choose which diet to use? This will depend on several factors, including; the patients’ circumstances, preferences, current intake, clinical condition and access to prescription products. Whichever diet is started, it will be optimised and fine tuned using a variety of strategies to support positive changes in both seizure and non seizure related outcomes.
Conditions typically treated with medical KD therapy
Epilepsy
Ketogenic diet (KD) therapy has been used since the 1920s to treat epilepsy. It is a well-established treatment for drug-resistant (difficult to treat) epilepsy in children and adults, with an ever-increasing number of randomised controlled trials demonstrating positive effects on seizure control. In general, approximately 50-60% of children will have 50% or more reduction in seizures, of whom 15% will become seizure free. In adults, approximately40-50% of achieve a 50% or more reduction in seizures, and 13% gain seizure freedom. Improvements in sleep, quality of life, behaviour and cognition are also reported. Patients should be referred for consideration of KD therapy when two or more anti-seizure medications have failed to control their seizures.
Neurometabolic diseases
Ketogenic diet is currently the only available treatment for two complex, rare metabolic diseases that affect brain energy metabolism: glucose transporter type 1 deficiency syndrome (GLUT1DS) and pyruvate dehydrogenase deficiency (PDH) syndrome. It provides ketones as an essential alternative fuel.
Migraines and headache disorders
Among the most prevalent and debilitating neurological disorders are headaches, and the ketogenic diet has been shown to reduce the frequency, duration and severity of headache episodes as well as the need for medication.
Research is ongoing to assess the role ketogenic diets may play in a range of other neurological disorders including brain tumours, Alzheimer’s, autism and psychiatric disorders.



